RESEARCH PAPER
The reversed Birth Satisfaction Scale: translation, adaptation and validation for a Greek sample
1
Midwifery Department of Athens, Technological Educational Institute of Athens, Athens, Greece
Submission date: 2017-04-17
Final revision date: 2017-08-21
Acceptance date: 2017-08-24
Publication date: 2017-09-20
Corresponding author
Victoria G. Vivilaki
Midwifery Department of Athens, Technological Educational Institute of Athens, Passionos 44-46, 11631 Athens, Greece
Midwifery Department of Athens, Technological Educational Institute of Athens, Passionos 44-46, 11631 Athens, Greece
Eur J Midwifery 2017;1(September):3
KEYWORDS
TOPICS
ABSTRACT
Introduction:
The Birth Satisfaction Scale (BSS) is an important screening instrument that is used with mothers during the postpartum period for the identification of postnatal birth satisfaction. The purpose of this study was to validate and adapt the Greek version of the BSS to test its sensitivity, specificity and predictive values.
Methods:
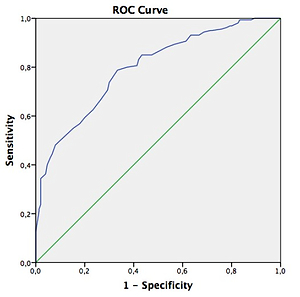
Childbearing women (n=310) were recruited from the perinatal care registers of the Maternity Departments of 3 Hospitals of Athens municipality (public Maternity Departments) in 2014. Inclusion criteria included fluency in spoken and written Greek language, within 1-4 postpartum days, and delivery of a healthy infant. Exploratory Factor Analysis (EFA) on the 30-items on the BSS revealed 7 orthogonal factors (KMO measure of sampling adequacy=0.856 and Bartlett’s test of sphericity=2999.806, df=435, p<0.0005). A Receiver Operating Characteristic (ROC) analysis was conducted to evaluate global functioning of the scale. Within this context the scoring of the BSS was reversed from the original, to indicate that a lower score was a worse outcome.
Results:
The Greek BSS showed high overall internal consistency (Cronbach’s alpha value: 0.876, p<0.0001). The internal consistency characteristics of the Greek BSS showed good reliability: Cronbach’s alpha was 0.876 for the total scale (Items 1-30), Standardized alpha 0.859 and Guttman split-half 0.864, Spearman-Brown 0.866. Our findings confirm the multidimensionality of BSS, demonstrating a seven-factor structure that contained subscales, reflecting the postnatal birth satisfaction. Exploratory Factor Analysis (EFA) demonstrated that the 7-factor model offered a very good fit to our data. The area under the minor satisfaction ROC curve is 0.796 (SD=0.025, Asymp. Sig.=0.0005; CI=0.748-0.845), sensitivity=73.8%, and specificity=70%.
Conclusions:
Our data confirm the validity of the Greek version of the BSS at identifying postnatal birth satisfaction. Hence, the Greek BSS could be used as a useful instrument in both clinical practice and research.
The Birth Satisfaction Scale (BSS) is an important screening instrument that is used with mothers during the postpartum period for the identification of postnatal birth satisfaction. The purpose of this study was to validate and adapt the Greek version of the BSS to test its sensitivity, specificity and predictive values.
Methods:
Childbearing women (n=310) were recruited from the perinatal care registers of the Maternity Departments of 3 Hospitals of Athens municipality (public Maternity Departments) in 2014. Inclusion criteria included fluency in spoken and written Greek language, within 1-4 postpartum days, and delivery of a healthy infant. Exploratory Factor Analysis (EFA) on the 30-items on the BSS revealed 7 orthogonal factors (KMO measure of sampling adequacy=0.856 and Bartlett’s test of sphericity=2999.806, df=435, p<0.0005). A Receiver Operating Characteristic (ROC) analysis was conducted to evaluate global functioning of the scale. Within this context the scoring of the BSS was reversed from the original, to indicate that a lower score was a worse outcome.
Results:
The Greek BSS showed high overall internal consistency (Cronbach’s alpha value: 0.876, p<0.0001). The internal consistency characteristics of the Greek BSS showed good reliability: Cronbach’s alpha was 0.876 for the total scale (Items 1-30), Standardized alpha 0.859 and Guttman split-half 0.864, Spearman-Brown 0.866. Our findings confirm the multidimensionality of BSS, demonstrating a seven-factor structure that contained subscales, reflecting the postnatal birth satisfaction. Exploratory Factor Analysis (EFA) demonstrated that the 7-factor model offered a very good fit to our data. The area under the minor satisfaction ROC curve is 0.796 (SD=0.025, Asymp. Sig.=0.0005; CI=0.748-0.845), sensitivity=73.8%, and specificity=70%.
Conclusions:
Our data confirm the validity of the Greek version of the BSS at identifying postnatal birth satisfaction. Hence, the Greek BSS could be used as a useful instrument in both clinical practice and research.
REFERENCES (42)
1.
Ware J. 1994. Monitoring health care from the patient’s point of view, Hospital Practice 15, 12-17.
doi: 10.1080/21548331.1994.11443012
2.
Mahon, P.Y. 1996. An analysis of the concept ‘patient satisfaction as it relates to contemporary nursing care”, Journal of Advanced Nursing, Vol. 24, pp. 1241-8.
doi: 10.1111/j.1365-2648.1996.tb01031.x
3.
Dannenbring, D., Stevens, M.J. and House, A.E. 1997. Predictors of childbirth pain and maternal satisfaction, Journal of Behavioural Medicine, Vol. 20 No. 2, pp. 127-42. doi: 10.1023/a:1025526610524
4.
Gibbens, J., Thomson, A. 2001. Women’s expectations and experiences of childbirth. Midwifery. Vol. 17, pp. 302-13. doi: 10.1054/midw.2001.0263
5.
Lomas J, Dore S, Enkin M, Mitchell A: The labor and delivery satisfaction index–the development and evaluation of a soft outcome measure. Birth1987,14:125–129. doi: 10.1111/j.1523-536x.1987.tb01472.x
6.
Sawyer et al. (2013) Measures of satisfaction with care during labour and birth: a comparative review. BMC Pregnancy and Childbirth 2013: 13 :108. doi: 10.1186/1471-2393-13-108
7.
Hollins Martin, C., Fleming V. 2009. The birth satisfaction scale. International Journal of Health Care. 24:124-135. doi: 10.1108/09526861111105086
8.
Hollins Martin, C., Martin, C.R. 2014. Development and psychometric properties of the Birth Satisfaction Scale-Revised (BSS-R). Midwifery. 30: 610–619. doi: 10.1016/j.midw.2013.10.006
9.
Barbosa-Leiker C., Hollins Martin CJ., Martin CR. (2015) Psychometric properties of the Birth Satisfaction Scale-Revised (BSS-R) for US mothers. Journal of Reproductive and Infant Psychology. 33(5):504-511. doi: 10.1080/02646838.2015.1024211
10.
Vardavaki Z., Hollins Martin CJ., Martin C. (2015). Construct and content validity of the Greek version of the Birth Satisfaction Scale (G-BSS). Journal of Reproductive and Infant Psychology. 33(5), 488-503. doi: 10.1080/02646838.2015.1035235
11.
Bowling A. 2002. Research Methods in Health: Investigating health and health services, 2nd edn, Maidenhead England: Open University Press. doi: 10.7748/nr.10.2.81.s11
12.
Hollins Martin, C., Snowden, A., Martin, C.R. 2012. Concurrent analysis: validation of the domains within the Birth Satisfaction Scale. Journal of Reproductive and Infant Psychology. 1-14. doi: 10.1080/02646838.2012.710833
13.
Tabachnick B., Fidell L. 2007. Using multivariate statistics. 3rd ed. N.Y.: Addison- Wesley- Longman.
14.
Kaiser, HF., 1960. The application of electronic computers to factor analysis. Educational and Psychological Measurement, (20) 141-151. doi: 10.1177/001316446002000116
15.
Hakstian A. R., Rogers W.D. & Cattell R.B. 1982. The behaviour of numbers factors rules with simulated data. Multivariate Behavioral Research 17, 193-219. doi: 10.1207/s15327906mbr1702_3
16.
Morrison, D.F. 1976. Multivariate statistical methods (2nd edition) New York, McGraw-Hill. doi: 10.1002/bimj.19700120121
17.
Geissbuehler V., Eberhard, J. 2002. Fear of childbirth during pregnancy: a study of more than 8000 pregnant women. J. Psychosom. Obstet. Gynecol. 23, 229–235. doi: 10.3109/01674820209074677
18.
McKenzie-McHarg K., 2004. Traumatic birth: understanding predictors, triggers, and counseling process is essential to treatment. Birth 31, 219–221. doi: 10.1111/j.0730-7659.2004.00308.x
19.
Beck, C.T. 2009. Birth trauma and its sequelae. J. Trauma Dissociation 10, 189–203. doi: 10.1080/15299730802624528
20.
Sorenson D.S., Tschetter, L. 2010. Prevalence of negative birth perception, disaffirmation, perinatal trauma symptoms, and depression among postpartum women. Perspect. Psychiatr. Care 46, 14–25. doi: 10.1111/j.1744-6163.2009.00234.x
21.
Brown S., Lumley, J. 1994. Satisfaction with care in labour and birth: a survey of 790 Australian women. Birth 21, 4–13. doi: 10.1111/j.1523-536x.1994.tb00909.x
22.
Niven C., Gijsbers K. 1984. A study of labor pain using the McGill pain questionnaire. Soc. Sci. Med. 19, 1347–1351. doi: 10.1016/0277-9536(84)90023-6
24.
Scott-Palmer J., Skevington, S.M. 1981. Pain during childbirth and locus of control. J. Psychosom. Res. 25, 151–155. doi: 10.1016/0022-3999(81)90027-1
25.
Handfield, B., Bell, R. 1995. Do childbirth preparation classes influence decision making about labour and postpartum issues? Birth 22, 153–160. doi: 10.1111/j.1523-536x.1995.tb00692.x
26.
Hall, S.M., Holloway, I.M. 1998. Staying in control: women's experiences of labour in water. Midwifery 14, 30–36. doi: 10.1016/s0266-6138(98)90112-7
27.
Melender H.L., 2002. Fears and coping strategies associated with pregnancy and childbirth in Finland. J. Midwifery Womens Health 47, 256–263. doi: 10.1016/s1526-9523(02)00263-5
28.
Halldorsdottir S., Karlsdottir, S.I. 1996. Journeying through labour and delivery: perceptions of women who have given birth. Midwifery 12, 48–61. doi: 10.1016/s0266-6138(96)90002-9
29.
Hodnett, E.D. 1996. Nursing support of the labouring woman. J. Obstet. Gynecol. Neonatal Nurs. 25, 257–264. doi: 10.1111/j.1552-6909.1996.tb02434.x
30.
Heaman M., Beaton, J.Gupton, A. 1992. A comparison of childbirth expectations in high risk and low risk pregnant women. Clin. Nurs. Res. 1, 252–265. doi: 10.1177/105477389200100305
31.
Wong N, Browne J, Ferguson S, Taylor J, Davis D (2015) Getting the first birth right: A retrospective study of outcomes for low-risk primiparous women receiving standard care versus midwifery model of care in the same tertiary hospital . Women and Birth 28 (2015) 279–284. doi: 10.1016/j.wombi.2015.06.005
32.
Sinclair M. 1999. The childbirth self-efficacy inventory: a replication study. J. Adv. Nurs. 30, 1416–1423. doi: 10.1046/j.1365-2648.1999.01230.x
33.
Proctor S. 1998. What determines quality in maternity care? Comparing the perceptions of childbearing women and midwives. Birth 25, 85–93. doi: 10.1046/j.1523-536x.1998.00085.x
34.
Stadlmayr W., Amsler F., Lemola S., et al. 2006. Memory of childbirth in the second year: the long term effect of a negative birth experience and its modulation by the perceived intranatal relationship with caregivers. J. Psychosom. Obstet. Gynecol. 27, 211–224. doi: 10.1080/01674820600804276
35.
Alehagen, S., Wijma, B. 2000. Can women's cognitive appraisal be registered throughout childbirth? Gynecol. Obstet. Invest. 49, 31–35. doi: 10.1159/000010209
36.
Wax J., Cartin, A., Pinette, M., Blackstone, J. 2004. Patient choice caesarean: an evidence based view. Obstet. Gynecol. Surv. 59, 601–616. doi: 10.1097/01.ogx.0000133942.76239.57
37.
Green, J.M., Baston, H.A., Easton, S.C, McCormick, F. 2003. Greater Expectations: The Inter-Relationship between Women's Expectations and Experience of Decision-Making, Continuity, Choice and Control in Labor, and Psychological Outcomes, Summary Report. Mother and Infant Research Unit (University of Leeds), Leeds.
38.
Goodman, P., Mackay, M.C., Tavakoli, A.S., 2004. Factors related to childbirth satisfaction. J. Adv. Nurs. 46, 212–219. doi: 10.1111/j.1365-2648.2003.02981.x
39.
Quine L., Rutter, D.R., Gowan, S. 1993. Women's satisfaction with the quality of the birth experience: a prospective study of social and psychological predictors. J. Reprod. Infant Psychol. 11, 107–113. doi: 10.1080/02646839308403202
40.
Melzack R., Taenzer, P., Feldman, P., Kinch, R. 1984. Labor is still painful after prepared childbirth. Can. Med. J. 125, 357–363. doi: 10.1016/0304-3959(81)90537-6
41.
Saisto et al (2001) Psychosocial predictors of disappointment with delivery and puerperal depression. A longitudinal study. Acta Obstet Gynecol Scand 2001; 80: 39–45. doi: 10.1080/791201832
42.
ICHOM (2017) Pregnancy and Childbirth data Collection Reference Guide. Version 1.0.3 Revised: April 10th, 2017.
CITATIONS (6):
1.
The Birth Satisfaction Scale: Igbo adaptation, validation, and reliability study
Chidebe Anikwe, Umeononihu Osita, Paul Mbanefo, Obiora Asiegbu, Ugochukwu Nnadozie, George Eleje, Arinze Ikeotuonye, Cyril Ikeoha, Charles Maduba, Justus Eze
Chidebe Anikwe, Umeononihu Osita, Paul Mbanefo, Obiora Asiegbu, Ugochukwu Nnadozie, George Eleje, Arinze Ikeotuonye, Cyril Ikeoha, Charles Maduba, Justus Eze
2.
The Birth Satisfaction Scale: Igbo adaptation, validation, and reliability study
Chidebe Anikwe, Umeononihu Osita, Paul Mbanefo, Obiora Asiegbu, Ugochukwu Nnadozie, George Eleje, Arinze Ikeotuonye, Cyril Ikeoha, Charles Maduba, Justus Eze
Chidebe Anikwe, Umeononihu Osita, Paul Mbanefo, Obiora Asiegbu, Ugochukwu Nnadozie, George Eleje, Arinze Ikeotuonye, Cyril Ikeoha, Charles Maduba, Justus Eze
3.
Adequate cardiorespiratory fitness during pregnancy for a better quality of childbirth
Roikhatul Jannah, Budi Utomo, Liza Laela Abida, Bimo Kholifah, Ahmad Syafiq, Wahyuddin Wahyuddin, Zahra Sativani
Healthcare in Low-resource Settings
Roikhatul Jannah, Budi Utomo, Liza Laela Abida, Bimo Kholifah, Ahmad Syafiq, Wahyuddin Wahyuddin, Zahra Sativani
Healthcare in Low-resource Settings
4.
The level of satisfaction with the experience of childbirth
Bohdana Dušová, Juliana Furčak, Radka Bužgová
Pielegniarstwo XXI wieku / Nursing in the 21st Century
Bohdana Dušová, Juliana Furčak, Radka Bužgová
Pielegniarstwo XXI wieku / Nursing in the 21st Century
5.
The birth satisfaction scale: Igbo adaptation, validation, and reliability study
Chidebe Christian Anikwe, Osita Samuel Umeononihu, Ifeyinwa Helen Anikwe, Arinze Chidiebele Ikeotuonye, Cyril Chijioke Ikeoha, Obiora GK Asiegbu, Justus Ndulue Eze, Ugochukwu Uzodimma Nnadozie, Charles Chidiebele Maduba, Mbanefo Paul Okeke, George Uchenna Eleje
BMC Pregnancy and Childbirth
Chidebe Christian Anikwe, Osita Samuel Umeononihu, Ifeyinwa Helen Anikwe, Arinze Chidiebele Ikeotuonye, Cyril Chijioke Ikeoha, Obiora GK Asiegbu, Justus Ndulue Eze, Ugochukwu Uzodimma Nnadozie, Charles Chidiebele Maduba, Mbanefo Paul Okeke, George Uchenna Eleje
BMC Pregnancy and Childbirth
6.
Adaptation and validation of the Polish version of the Quality from Patient Perspective - Intrapartal (QPP-I) questionnaire to assess childbirth care
Julia Nawrot, Dorota Matuszyk, Aneta Suder, Agnieszka Bień, Violetta Skrzypulec-Plinta, Agnieszka Gniadek
European Journal of Midwifery
Julia Nawrot, Dorota Matuszyk, Aneta Suder, Agnieszka Bień, Violetta Skrzypulec-Plinta, Agnieszka Gniadek
European Journal of Midwifery
Share
RELATED ARTICLE
We process personal data collected when visiting the website. The function of obtaining information about users and their behavior is carried out by voluntarily entered information in forms and saving cookies in end devices. Data, including cookies, are used to provide services, improve the user experience and to analyze the traffic in accordance with the Privacy policy. Data are also collected and processed by Google Analytics tool (more).
You can change cookies settings in your browser. Restricted use of cookies in the browser configuration may affect some functionalities of the website.
You can change cookies settings in your browser. Restricted use of cookies in the browser configuration may affect some functionalities of the website.