STUDY PROTOCOLS
Midwives’ contribution to normal childbirth care: Cross-sectional study in public health settings, the MidconBirth Study protocol
1
Mar Shool of Nursing, Mar School of Nursing. University Pompeu Fabra, Barcelona, Spain
2
Hospital Parc de Salut Mar. Barcelona, Spain
3
Department of Experimental and Health Sciences. University Pompeu Fabra. Barcelona, Spain
4
Hospital Universitari Vall d’Hebron, Barcelona, Spain
5
Departament de Ciències de la Salut. Universitat de Vic-Universitat Central de Catalunya, Barcelona, Spain
6
Mar School of Nursing. University Pompeu Fabra. Barcelona, Spain
7
University of Central Lancashire. School of Community Health and Midwifery, UK
8
Department of Health Services Research. The University of Liverpool, Liverpool, UK
9
School of Nursing and Midwifery. Trinity College Dublin, Ireland
Submission date: 2017-03-23
Final revision date: 2017-09-04
Acceptance date: 2017-09-04
Publication date: 2017-09-21
Corresponding author
Ramón Escuriet
Mar Shool of Nursing, Mar School of Nursing. University Pompeu Fabra, Doctor Aiguader, 80, 3ª Planta (Despatx 61.311), 08003 Barcelona, Spain
Mar Shool of Nursing, Mar School of Nursing. University Pompeu Fabra, Doctor Aiguader, 80, 3ª Planta (Despatx 61.311), 08003 Barcelona, Spain
Eur J Midwifery 2017;1(September):4
KEYWORDS
TOPICS
ABSTRACT
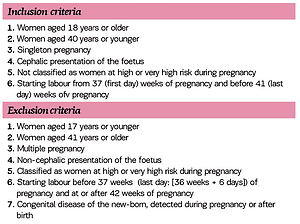
This paper presents the Protocol for a multicentre study that seeks to analyse the relationship between midwife care during childbirth and spontaneous vaginal birth. Each participating hospital collects outcome data from a sample of all women birthing, determined according to the number of annual births attended by midwives, in each hospital.
Data collected are sociodemographic variables (age, nationality, level of education). Clinical variables collected are onset of labour, augmentation of labour, professional (midwife or obstetrician) providing care in the first and second stage of labour, transfer of care between professionals, mobility during labour, pharmacological and non-pharmacological pain-management methods used, if any, position for birth, mode of birth outcomes, Apgar score at 1 and 5 minutes, birth weight, timing of breastfeeding initiation and breastfeeding rates. The Bologna Score scale items, are evaluated also.
The midwife’s contribution in the care of normal birth, and the relationship with spontaneous birth (i.e. vaginal birth without the use of instruments) will serve as a basis for further improving the quality of care provided to pregnant women and their families. Phase I of the study ended in January 2017.
REFERENCES (12)
1.
Sandall J, Soltani H, Gates S, Shennan A, Devane D. Midwife led continuity models versus other models of care for childbearing women. Cochrane Database of Systematic Reviews 2013, Issue 8. Art. No.: CD004667. doi: 10.1002/14651858.cd004667.pub3
2.
Kenny Christopher, Devane Declan, Normand Charles, Clarke Mike, Howard Aoife, Begley Cecily. A cost-comparison of midwife-led compared with consultant-led maternity care in Ireland (the MidU study). Midwifery. 31(11):1032-8; 2015. doi: 10.1016/j.midw.2015.06.012
3.
Delgado Nunes V., Gholitabar M., Sims J. M., Bewley S.. Intrapartum care of healthy women and their babies: summary of updated NICE guidance. BMJ: British Medical Journal. 2014, 349. doi: 10.1136/bmj.g6886
4.
The American College of Obstetricians and gynecologists. Approaches to limit interventions during labor and birth Committee opinion. Feb 2017. Number 687.
5.
Lewis, Debrah, and Soo Downe. "FIGO consensus guidelines on intrapartum fetal monitoring: Intermittent auscultation." International Journal of Gynecology & Obstetrics. 2015. 131(1) : 9-12. doi: 10.1016/j.ijgo.2015.06.019
6.
Miller Suellen, Abalos Edgardo, Chamillard Monica, Ciapponi Agustin, Colaci Daniela, Comandé Daniel, Diaz Virginia, Geller Stacie, Hanson Claudia, Langer Ana, Manuelli Victoria, Millar Kathryn, Morhason-Bello Imran, Castro Cynthia Pileggi, Pileggi Vicky Nogueira, Robinson Nuriya, Skaer Michelle, Souza João Paulo, Vogel Joshua P, Althabe Fernando. "Beyond too little, too late and too much, too soon: a pathway towards evidence-based, respectful maternity care worldwide." The Lancet. 2016; 388: 2176-2192. doi: 10.1016/s0140-6736(16)31472-6
7.
Bernal Delgado E, Aibar Remón C, Villaverde Royo MV, Abadía Taira MB, Martínez N, Librero López J, et al. Variaciones en la utilización de cesárea en los hospitales públicos del Sistema Nacional de Salud [internet]. [Zaragoza]: VMP. Atlas de Variaciones en la Práctica Médica en el Sistema Nacional de Salud; 2009 [Internet]. Documento de trabajo: 04/2009. Available in: http://www.atlasvpm.org/avpm/n....
8.
Maceiras Rozas MC, Salgado Barreira A, Atienza Merino G. La asistencia al parto de las mujeres sanas. Estudio de la variabilidad y revisión sistemática. Madrid: Ministerio de Ciencia e Innovación; 2009. doi: 10.1016/j.pog.2010.01.003
9.
Devane D, Murphy-Lawless J, Begley CM. Childbirth policies and practices in Ireland and the journey towards midwifery-led care. Midwifery. 23(1);92-101; 2007. doi: 10.1016/j.midw.2005.08.006
10.
Chalmers Beverley, Porter Richard. Assessing the effective care in normal labour: The Bologna Score. Birth 28:2; June 2001. doi: 10.1046/j.1523-536x.2001.00079.x
11.
Kozhimannil B.K, Law M.R, Virnig B.A. Cesarean delivery rates vary tenfold among US hospitals; Reducing variation may address quality and cost issues. Health Affairs, 32, no.3:527-535; 2013. doi: 10.1377/hlthaff.2012.1030
12.
Kenny Christopher, Devane Declan, Normand Charles, Clarke Mike, Howard Aoife, Begley Cecily. A cost-comparison of midwife-led compared with consultant-led maternity care in Ireland (the MidU study). Midwifery. 31(11):1032-8; 2015. doi: 10.1016/j.midw.2015.06.012
CITATIONS (5):
1.
Relation between Epidural Analgesia and severe perineal laceration in childbearing women in Catalonia
L. Garcia-Lausin, M. Perez-Botella, X. Duran, S. Rodríguez-Pradera, M.J. Gutierrez-Martí, R. Escuriet
Midwifery
L. Garcia-Lausin, M. Perez-Botella, X. Duran, S. Rodríguez-Pradera, M.J. Gutierrez-Martí, R. Escuriet
Midwifery
2.
Relation between Length of Exposure to Epidural Analgesia during Labour and Birth Mode
Laura Garcia-Lausin, Mercedes Perez-Botella, Xavier Duran, Maria Mamblona-Vicente, Maria Gutierrez-Martin, de Gómez, Ramon Escuriet
International Journal of Environmental Research and Public Health
Laura Garcia-Lausin, Mercedes Perez-Botella, Xavier Duran, Maria Mamblona-Vicente, Maria Gutierrez-Martin, de Gómez, Ramon Escuriet
International Journal of Environmental Research and Public Health
3.
Transfers of Care between Healthcare Professionals in Obstetric Units of Different Sizes across Spain and in a Hospital in Ireland: The MidconBirth Study
Anna Martín-Arribas, Rafael Vila-Candel, Rhona O’Connell, Martina Dillon, Inmaculada Vila-Bellido, M. Beneyto, Molina-Fernández De, Nerea Rodríguez-Conesa, Cristina González-Blázquez, Ramón Escuriet
International Journal of Environmental Research and Public Health
Anna Martín-Arribas, Rafael Vila-Candel, Rhona O’Connell, Martina Dillon, Inmaculada Vila-Bellido, M. Beneyto, Molina-Fernández De, Nerea Rodríguez-Conesa, Cristina González-Blázquez, Ramón Escuriet
International Journal of Environmental Research and Public Health
4.
A comparison between midwifery and obstetric care at birth in Spain: Across-sectional study of perinatal outcomes
Anna Martin-Arribas, Ramon Escuriet, Alicia Borràs-Santos, Rafael Vila-Candel, Cristina González-Blázquez
International Journal of Nursing Studies
Anna Martin-Arribas, Ramon Escuriet, Alicia Borràs-Santos, Rafael Vila-Candel, Cristina González-Blázquez
International Journal of Nursing Studies
5.
Midwife-attended planned home births versus planned hospital births in Spain: Maternal and neonatal outcomes
Lucia ALCARAZ-VIDAL, Ramon ESCURIET, Roser PALAU-COSTAFREDA, Fatima LEON-LARIOS, Gemma ROBLEDA
Midwifery
Lucia ALCARAZ-VIDAL, Ramon ESCURIET, Roser PALAU-COSTAFREDA, Fatima LEON-LARIOS, Gemma ROBLEDA
Midwifery
Share
RELATED ARTICLE
We process personal data collected when visiting the website. The function of obtaining information about users and their behavior is carried out by voluntarily entered information in forms and saving cookies in end devices. Data, including cookies, are used to provide services, improve the user experience and to analyze the traffic in accordance with the Privacy policy. Data are also collected and processed by Google Analytics tool (more).
You can change cookies settings in your browser. Restricted use of cookies in the browser configuration may affect some functionalities of the website.
You can change cookies settings in your browser. Restricted use of cookies in the browser configuration may affect some functionalities of the website.