Home
Archive of Issues
Aim & Scope
Open Access
Supporting Midwifery Associations
Indexing
Why publish with us
Contact us
Editorial Board
Instructions to Authors (PDF)
Manuscript Types
Manuscript Formatting
How to submit
Preprints
Professional Editing Service
Authorship & COI
Principles of Transparency Checklist
Publication Ethics and Publication Malpractice Statement
CrossMark
Data Policies
Supporting Diversity
Social Media
RESEARCH PAPER
The fluid balance observed postnatally on normal pregnancies, pregnancies with preeclampsia, and on pregnancies with oedema and proteinuria
1
Department of Midwifery, Technological Educational Institute of Athens, Greece
2
Pulmonary Department, Intensive Care Medicine, Evaggelismos Hospital, Medical School, University of Athens, Athens, Greece
Submission date: 2017-04-28
Final revision date: 2017-10-26
Acceptance date: 2017-12-01
Publication date: 2017-12-18
Corresponding author
Athina Diamanti
Department of Midwifery, Technological Educational Institute of Athens, Greece, Tzermia 6, 15121 Pefki, Greece
Department of Midwifery, Technological Educational Institute of Athens, Greece, Tzermia 6, 15121 Pefki, Greece
Eur J Midwifery 2017;1(December):6
KEYWORDS
TOPICS
ABSTRACT
Introduction:
It is observed that delivery does not completely eliminate the risk of developing symptoms of preeclampsia, as well as its impending complications. The postpartum period is often associated with a high risk of developing preeclampsia, eclampsia and HELLP syndrome. Yet, there is neither an established standard, nor specific guidelines for peripartum fluid management. Our purpose is to study during the first four days of the postpartum period the differences in fluid balance on: normal pregnancies, pregnancies with preeclampsia and pregnancies with oedema and proteinuria.
Methods:
The setting was the Gaia private maternity clinic in Athens, where 100 women in the postpartum period took part in the study and were requested to fill in a data collection-sheet, specially developed for the study. They were recruited between January 2014 and November 2014 and were divided into three groups. Group I consisted of all normal pregnancies, Group II those with oedema and proteinuria, and Group III those with preeclampsia. The demographic and clinical characteristics of the women and fetuses were initially recorded. Subsequently, daily records of fluid balance, as well as body weight, were kept for four days after labor. Descriptive statistics were used to analyze the demographic data of the sampled women. We compared the fluid balances among the three groups using t-test association and one-way Anova.
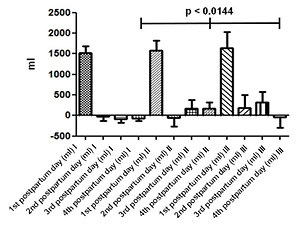
Results:
The mean age of the women was 32.48±4.38 years. Out of a total of 100 women, 59 of them had a normal pregnancy (Group I), 24 developed oedema and proteinuria (Group II) and 17 developed preeclampsia (Group III). All three groups had a positive fluid balance on the first day postpartum and only the first group had a negative cumulative fluid balance from the second day postpartum and onwards. The second group despite having started to discard a small volume of fluid, from the second day postpartum, the balance remained positive throughout the next two days. The third group however, had a negative fluid balance only during the fourth day after labor.
Conclusions:
ur results indicate a difference in the kinetics of fluids in women with preeclampsia, compared to those that had a normal pregnancy and postpartum period. Consequently, there appears to be a need for more rational management and follow up on fluid balance throughout labor.
It is observed that delivery does not completely eliminate the risk of developing symptoms of preeclampsia, as well as its impending complications. The postpartum period is often associated with a high risk of developing preeclampsia, eclampsia and HELLP syndrome. Yet, there is neither an established standard, nor specific guidelines for peripartum fluid management. Our purpose is to study during the first four days of the postpartum period the differences in fluid balance on: normal pregnancies, pregnancies with preeclampsia and pregnancies with oedema and proteinuria.
Methods:
The setting was the Gaia private maternity clinic in Athens, where 100 women in the postpartum period took part in the study and were requested to fill in a data collection-sheet, specially developed for the study. They were recruited between January 2014 and November 2014 and were divided into three groups. Group I consisted of all normal pregnancies, Group II those with oedema and proteinuria, and Group III those with preeclampsia. The demographic and clinical characteristics of the women and fetuses were initially recorded. Subsequently, daily records of fluid balance, as well as body weight, were kept for four days after labor. Descriptive statistics were used to analyze the demographic data of the sampled women. We compared the fluid balances among the three groups using t-test association and one-way Anova.
Results:
The mean age of the women was 32.48±4.38 years. Out of a total of 100 women, 59 of them had a normal pregnancy (Group I), 24 developed oedema and proteinuria (Group II) and 17 developed preeclampsia (Group III). All three groups had a positive fluid balance on the first day postpartum and only the first group had a negative cumulative fluid balance from the second day postpartum and onwards. The second group despite having started to discard a small volume of fluid, from the second day postpartum, the balance remained positive throughout the next two days. The third group however, had a negative fluid balance only during the fourth day after labor.
Conclusions:
ur results indicate a difference in the kinetics of fluids in women with preeclampsia, compared to those that had a normal pregnancy and postpartum period. Consequently, there appears to be a need for more rational management and follow up on fluid balance throughout labor.
REFERENCES (23)
1.
CheungK.L. Lafayette R.A. Renal Physiology of Pregnancy. Advances in Chronic Kidney Disease . 2013;20(3): 209-14. doi: 10.1053/j.ackd.2013.01.012.
2.
Hunter S., RobsonS.C. Adaptation of the maternal heart in pregnancy. BrHeart J 1992;68, 540-543. doi: 10.1136/hrt.68.12.540
3.
Horowitz K.M., IngardiaC.J., BogidaA.F. Anemia in pregnancy. Clinics in Laboratory Medicine 2013;33, 281-291. doi: 10.1016/j.cll.2013.03.016.
4.
Adamova Z., Ozkan S., Khalil R.A. Vascular and Cellular Calcium in Normal and Hypertensive Pregnancy. Current Clinical Pharmacology 2009;4, 172–190. doi:10.2174/157488409789375320
5.
Bridges E.J., WombleS., WallaceM., McCartneyJ. Hemodynamic Monitoring in High-Risk Obstetrics Patients I.Critical Care Nurse 2003; 23, 53-62.
6.
Morton A. Primary aldosteronism and pregnancy. Pregnancy hypertension. Received: August 1, 2015; Accepted: August 11, 2015; Published Online: August 12, 2015. doi: 10.1016/j.preghy.2015.08.003.
7.
National Institute for health and Care Excellence (NICE), Hypertension in pregnancy: The management of hypertensive disorders during pregnancy. NICE clinical guidelines, No. 107. RCOG Press; 2010 Aug.
8.
The American College Of obstetricians and Gynecologists. The diagnosis and management of preeclampsia and eclampsia clinical practice guideline. Version 1.0 Guideline No. 3 Date of publication – September 2011 Revision date – September 2013.
9.
Magee L.A., Pels A. , Helewa M. , Rey E., von Dadelszen P. Diagnosis, evaluation, and management of the hypertensive disorders of pregnancy: executive summary. Canadian Hypertensive Disorders of Pregnancy Working Group. J Obstet Gynaecol Can. 2014 May;36(5):416-41. doi: 10.1016/s1701-2163(15)30588-0
10.
Moran P, Lindheimer MD, Davison JM. The renal response to preeclampsia. Semin Nephrol. 2004 Nov;24(6):588-95. doi: 10.1016/j.semnephrol.2004.07.008
11.
Turner J.A. Severe Preeclampsia: Anesthetic Implications of the Disease and Its Management. American Journal of Therapeutics 2009;16, 284-288. doi: 10.1097/mjt.0b013e31816f6fd8
12.
Cipolla M.J., Kraig R.P. Seisures in women with preeclampsia: Mechanisms and management. Fetal and Maternal Medicine Review 2011;22, 91-108. doi: 10.1017/S0965539511000040
13.
SibaiB.M., Mabie W.C. Hemodynamics of preeclampsia. Clinical Perinatology 1991;18, 727-747.
14.
Matthys LA, Coppage KH, Lambers DS, Barton JR, Sibai BM. Delayed postpartum preeclampsia: an experience of 151 cases. Am J Obstet Gynecol. 2004 May;190(5):1464-6. doi: 10.1016/j.ajog.2004.02.037
15.
Chames M.C., Livingston J.C., Ivester T.S., Barton J.R., Sibai B.M. Late postpartum eclampsia: a preventable disease? Am J Obstet Gynecol. 2002 Jun;186(6):1174-7. doi: 10.1067/mob.2002.123824
16.
Brady W.J, DeBehnkeD.J., Carter C.T. Postpartum toxemia : hypertension, edema, proteinuria and unresponsiveness in an unknown female. Journal of Emergency Medicine 1995;13, 643-648.
doi: 10.1016/0736-4679(95)00070-q
17.
Mackenzie M.J., Woolnough M.J., Barrett N., Johnson M.R., YentisS.M. Normal urine output after elective caesarean section: an observational study. International Journal of Obstetric Anesthesia 2010;19, 379–383. doi: 10.1016/j.ijoa.2010.06.005.
18.
Ickx B.E. Fluid and blood transfusion management in obstetrics. European Journal of Anaesthesiology 2010;27, 1031-1035. doi: 10.1097/EJA.0b013e32833c30e3.
19.
EngelhardtT., MacLennan F.M. Fluid management in pre-eclampsia. International Journal of Obstetric Anesthesia 1999;8, 253-259. doi: 10.1016/s0959-289x(99)80106-x.
20.
Pouta A.M., Räsänen J.P., Airaksinen K.E., Vuolteenaho O.J., Laatikainen T.J. Changes in maternal heart dimensions and plasma atrial natriuretic peptide levels in the early puerperium of normal and pre-eclamptic pregnancies. British Journal of Obstetrics and Gynaecology 1996;103, 988-992. doi: 10.1111/j.1471-0528.1996.tb09548.x.
21.
Al-Takroni A.M., Parvathi C.K., Mendis K.B., Hassan S., Qunaibi A.M. Early oral intake after caesarean section performed under general anaesthesia. Journal of Obstetrics and Gynaecology 1999;19, 34–37. doi: 10.1080/01443619965921.
22.
Joo K.W., Jeon U.S., Kim G.H., Park J., Oh Y.K., Kim Y.S., Ahn C., Kim S., Kim S.Y., Lee J.S., Han J.S. Antidiuretic action of oxytocin is associated with increased urinary excretion of aquaporin-2. Nephrol Dial Transplant 2004;19, 2480-2486. doi: 10.1093/ndt/gfh413.
23.
Bungum L., Tollan A., Oian P. Antepartum to postpartum changes in transcapillary fluid balance. British Journal of Obstetrics and Gynaecology 1990;97, 838-842. doi: 10.1111/j.1471-0528.1990.tb02580.x.
Share
RELATED ARTICLE
We process personal data collected when visiting the website. The function of obtaining information about users and their behavior is carried out by voluntarily entered information in forms and saving cookies in end devices. Data, including cookies, are used to provide services, improve the user experience and to analyze the traffic in accordance with the Privacy policy. Data are also collected and processed by Google Analytics tool (more).
You can change cookies settings in your browser. Restricted use of cookies in the browser configuration may affect some functionalities of the website.
You can change cookies settings in your browser. Restricted use of cookies in the browser configuration may affect some functionalities of the website.